Ten Key Points about External Radiation Therapy
- Radiation is a local, targeted therapy designed to kill cancer cells that may still exist after surgery. Radiation is given to the area where the cancer started or to another part of the body to which the cancer spread.
- The actual delivery of radiation treatment is painless. But the radiation itself may cause some discomfort over time.
- External radiation treatment, the most common kind of radiation therapy, does not make you radioactive.
- Treatment is usually given 5 days a week for up to 7 weeks. Sometimes radiation may be given twice a day for 1 week.
- Since the daily appointments usually take about 30 minutes, you’ll most likely be able to follow most of your normal routine during treatment.
- Radiation will not make you lose your hair, unless radiation is given to your head.
- In the area where you are receiving radiation, your skin can turn pink, red, or tan, and may be sensitive and irritated. Creams and other medicines can soothe these symptoms.
- During your treatment course, you may feel tired. This feeling can last for a few weeks—even months—after treatment ends.
- Most radiation side effects are temporary.
- Radiation therapy can significantly decrease the risk of cancer returning after surgery.
How Radiation Works
Radiation therapy uses a special kind of high-energy beam to damage cancer cells. (Other types of energy beams include light and X-rays.) These high-energy beams, which are invisible to the human eye, damage a cell’s DNA, the material that cells use to divide.
Over time, the radiation damages cells that are in the path of its beam—normal cells as well as cancer cells. But radiation affects cancer cells more than normal cells. Cancer cells are very busy growing and multiplying—2 activities that can be slowed or stopped by radiation damage. And because cancer cells are less organized than healthy cells, it’s harder for them to repair the damage done by radiation. So cancer cells are more easily destroyed by radiation, while healthy, normal cells are better able to repair themselves and survive the treatment.
There are two different ways to deliver radiation to the tissues to be treated:
- A machine called a linear accelerator that delivers radiation from outside the body. We use a very advanced linear accelerator called Tomotherapy, and you can learn more about this linear accelerator and its benefits in our web page.
- Pellets, or seeds, of material that give off radiation beams from inside the body. Dr. Grado is considered a pioneer in the use of this type of radiation for prostate cancer and has performed more than 6000 surgeries with excellent clinical results.
Tissues to be treated might include the breast area, lymph nodes, or another part of the body such as the prostate.
Some people may fear radiation therapy. They may worry that therapeutic radiation may be dangerous like an atomic bomb or nuclear power plant. Stories about radiation side effects, some of them exaggerated, can circulate around hospital waiting rooms. It’s important for you to know that there is NO connection between therapeutic radiation and the types of radiation in bombs and nuclear reactors. The radiation used in cancer treatment is highly focused, controllable, and generally safe.
Why Radiation is Necessary
Radiation is an important and often necessary form of anti-cancer therapy because it is able to reduce the risk of recurrence after surgery. Although it’s quite possible that your surgeon removed all the cancer, breast cancer surgery cannot guarantee that every cancer cell has been removed from your body.
Individual cancer cells are too small to be felt or seen during surgery or detected by testing. Any cells that remain after surgery can grow and eventually form a new lump or show up as an abnormality on a test such as a mammogram.
Research has shown that people who are treated with radiation after lumpectomy are more likely to live longer, and remain cancer-free longer, than those who don’t get radiation. In one large study, women who didn’t get radiation after lumpectomy were shown to have a 60% greater risk of the cancer coming back in the same breast. Other research has shown that even women with very small cancers (1 centimeter or smaller) benefit from radiation after lumpectomy.
Making a Plan after Prostate Cancer Diagnosis
Knowledge is power. The first step in making your plan is to ask questions—a lot of them. As you gather information, we will work with you and your loved ones to make a plan. Many things may be on your mind after you learn you have prostate cancer. You may also feel anxious or overwhelmed and wonder how you can cope during the days ahead. In addition to dealing with the diagnosis of cancer, you will learn a new language: that of prostate cancer and prostate cancer treatment.
Get the Facts about Your Cancer Diagnosis
Try to obtain as much basic, useful information as possible about your diagnosis. Consider bringing a family member or friend with you to your first few appointments. They can take notes and keep the new information organized.
- Learn about the stage, grade, and risk category of your disease.
- Ask about genetic tests that can predict aggressive or slow-growing prostate cancer.
- Find a doctor that makes you feel comfortable, answers your questions, and gives you confidence in treating your prostate cancer.
- Complete additional testing to determine if the cancer has spread and if so, how far. At Southwest Oncology Centers, we will help you understand.
- Find out about available clinical trials.
- Learn what side effects can be caused by each treatment offered and consider how they can affect your lifestyle.
Be Good to Yourself
- You are in control; a cancer diagnosis is only part of what defines you.
- Take time to think about what you want from your life.
- Connect with friends and family.
- Practice healthy eating habits by increasing fruits and vegetables and limit fats and alcohol.
- Don’t smoke.
- Get active—research has shown that exercise reduces death in male cancer survivors
We are glad to help you answer this and other questions you may have. Please give us a call at 480-614-6300 so you can talk to one of our physicians about your plan and treatment.
What is Your Prostate?
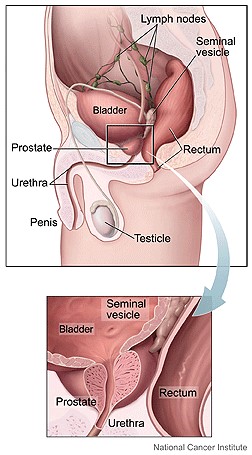
The prostate is a walnut-shaped gland in the male reproductive system that is located beneath the bladder and in front of the rectum. It surrounds the upper part of the urethra, which is the tube that carries urine from the bladder.
The size of the prostate varies with age. As a man ages, the prostate can grow larger.
The prostate has several important functions:
- Helps control urine flow, semen, and seminal fluid
- Essential for erections
- Produces seminal fluid to carry and nourish sperm
- Contains nerves needed to achieve an erection
- Provides the push sperm need to swim their way out of the penis
- Produces prostate specific antigen
The prostate is divided into lobes and zones. There are four lobes: anterior, median, lateral, and posterior. There are three zones: peripheral, central, and transitional. These terms refer to specific areas of the prostate to help the physician know where the cancer is located in the prostate.
Prostate Specific Antigen (PSA) is a substance produced by the prostate gland. It keeps semen in liquid form so sperm can swim. It is present in the bloodstream, and the level is a valuable piece of information in understanding a man’s prostate cancer risk, along with the digital rectal exam and other tests.
The level of PSA in a man’s blood can be a marker of many different prostate conditions, not only prostate cancer. The most frequent benign (non-cancerous) conditions that cause an elevation in PSA are the following:
- Prostatitis – inflammation of the prostate
- Benign Prostatic Hyperplasia (BHP) – enlargement of the prostate
Information Request Form
Please enter your name, email address and phone number where requested, and write a brief specific inquiry where designated. Before clicking the “SEND” button, please check the box to the left of “I’m not a robot” to verify that this email is coming from you rather than from an unauthorized email user.
